Nutriewind, Nutrition, Nutritionist Consultation
Epilepsy and Nutrition: How Diet Can Help Manage Seizures
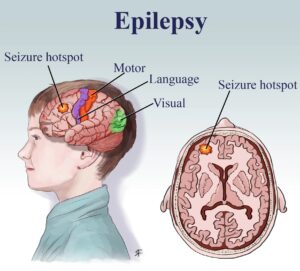
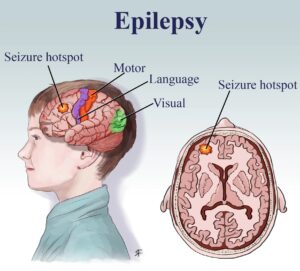
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures caused by abnormal electrical activity in the brain. It affects people of all ages and varies in severity. While medical treatments such as anti-epileptic drugs (AEDs) and surgery are commonly used, dietary interventions can also play a crucial role in managing epilepsy naturally.
Epilepsy and Nutrition
Causes of Epilepsy
Several factors contribute to epilepsy, including:
- Genetic Factors – Family history and inherited mutations.
- Head Injury – Trauma from accidents or falls.
- Brain Conditions – Stroke, tumors, or infections like meningitis.
- Prenatal Injury – Brain damage due to malnutrition or infections during pregnancy.
- Developmental Disorders – Conditions such as autism and neurofibromatosis.
Symptoms of Epilepsy
Common epilepsy symptoms include:
- Seizures – Can range from focal (affecting one part of the brain) to generalized (affecting the entire brain).
- Temporary Confusion – Feeling disoriented after a seizure.
- Staring Spells – Brief moments of unresponsiveness (common in absence seizures).
- Jerking Movements – Repetitive muscle twitches in hands and legs.
- Loss of Consciousness – Some seizures cause a complete loss of awareness.
- Psychological Symptoms – Anxiety or fear before or after seizures.

Epilepsy and Nutrition: How Diet Can Help Manage Seizures
Diagnosis of Epilepsy
Doctors use various methods to diagnose epilepsy, including:
- Medical History & Neurological Exams – Assessing brain function and symptoms.
- Electroencephalogram (EEG) – Monitoring brain waves for abnormal activity.
- Brain Imaging (MRI/CT Scan) – Detecting structural abnormalities.
- Blood Tests – Ruling out other conditions causing seizures.
Treatment Options for Epilepsy
Treatment for epilepsy depends on the type and severity of seizures. The most common options include:
- Anti-Epileptic Drugs (AEDs) – Medications to control seizures.
- Surgery – Removing the brain area causing seizures if medications fail.
- Vagus Nerve Stimulation (VNS) – A device that sends electrical signals to the brain.
- Responsive Neurostimulation (RNS) – A device that detects seizure activity and stimulates the brain to prevent seizures.
- Ketogenic Diet – A low-carb, high-fat diet that has shown promise in reducing seizures.

Epilepsy and Nutrition
The Role of Nutrition in Epilepsy Management
A well-balanced diet is essential in managing epilepsy and supporting brain health. The right dietary choices can help reduce seizure frequency and improve overall well-being.
Best Diets for Epilepsy
Several specialized diets can aid in seizure management, including:
1. Ketogenic Diet
The ketogenic diet is a high-fat, low-carbohydrate diet that forces the body into ketosis, where fat is used as the primary energy source instead of glucose. Studies suggest that this metabolic state may reduce seizure frequency, especially in drug-resistant epilepsy.
2. Modified Atkins Diet (MAD)
Similar to the ketogenic diet but more flexible, the Modified Atkins Diet (MAD) allows a broader range of foods while still maintaining a low carbohydrate intake. It is easier to follow and may help control seizures effectively.
3. Low Glycemic Index Treatment (LGIT)
The Low Glycemic Index Treatment (LGIT) focuses on consuming foods with a low glycemic index to stabilize blood sugar levels, which may help prevent seizures in some individuals.
Key Nutritional Principles for Epilepsy Management
- Consistency – Strict adherence to a prescribed diet ensures better seizure control.
- Adequate Nutrient Intake – Monitoring vitamins and minerals to prevent deficiencies due to dietary restrictions.
- Hydration – Staying properly hydrated, as dehydration can act as a seizure trigger.
- Avoiding Seizure Triggers – Limiting caffeine, alcohol, and processed foods known to trigger seizures in some people.
Final Thoughts
Managing epilepsy involves a combination of medical treatments and dietary interventions. The ketogenic diet, Modified Atkins Diet, and Low Glycemic Index Treatment have all shown promise in reducing seizure frequency. By incorporating a well-balanced diet rich in essential nutrients, individuals with epilepsy can enhance brain health and improve overall well-being.
If you or a loved one has epilepsy, consult with a healthcare professional or registered dietitian to determine the best nutrition plan for your needs.
Stay informed, stay healthy! For more expert nutrition tips, follow Nutriewind – your trusted source for evidence-based dietary guidance.

Nutrition
What is Insomnia?
Insomnia is a common sleep disorder that makes it difficult to fall asleep, stay asleep, or get quality rest. It can lead to daytime fatigue, mood disturbances, and poor health outcomes.
Types of Insomnia
- Primary Insomnia – Not linked to other health conditions.
- Secondary Insomnia – Caused by underlying medical issues like depression, asthma, arthritis, or medication.
- Sleep-Onset Insomnia – Trouble falling asleep.
- Sleep-Maintenance Insomnia – Difficulty staying asleep.
- Mixed Insomnia – Both sleep-onset and sleep-maintenance issues.
- Paradoxical Insomnia – Underestimating sleep duration.
Common Causes of Insomnia
Primary Causes:
- Stress from job loss, divorce, or a major life event
- Disruptive sleep environment (noise, light, or temperature changes)
- Jet lag or shift work
- Genetic predisposition to sleep disorders
Secondary Causes:
- Mental health conditions like anxiety or depression
- Medications (for allergies, asthma, high blood pressure, etc.)
- Pain, discomfort, or hormonal changes (pregnancy, menopause)
- Caffeine, alcohol, or nicotine consumption
- Sleep disorders like sleep apnea or restless leg syndrome
- Neurological conditions such as Alzheimer’s or ADHD
Complications of Insomnia
Long-term sleep deprivation can lead to severe health issues, including:
- High blood pressure
- Weakened immune system
- Increased risk of obesity, diabetes, and heart disease
- Cognitive decline and memory problems

Nutriewind- Best Nutrition & Dietician in Hyderabad
Best Ways to Prevent Insomnia
- Maintain a Consistent Sleep Schedule – Go to bed and wake up at the same time daily.
- Reduce Screen Time Before Bed – Avoid blue light from phones, tablets, and e-books.
- Limit Stimulants – Avoid caffeine, nicotine, and alcohol in the evening.
- Exercise Regularly – Engage in physical activity at least 3-4 hours before bedtime.
- Eat Light at Night – Avoid heavy meals close to bedtime but consider a light, sleep-friendly snack.
- Optimize Your Sleep Environment – Keep your bedroom dark, quiet, and at a comfortable temperature.
- Follow a Bedtime Routine – Wind down with reading, music, or a warm bath.
- Use Your Bed for Sleep Only – Avoid working or watching TV in bed.
- Manage Stress & Anxiety – Keep a journal or practice relaxation techniques before sleeping.
Best Foods for Better Sleep
Adding sleep-promoting foods to your diet can naturally improve sleep quality. Here are the top sleep-friendly foods:
- Almonds & Walnuts – Rich in melatonin, magnesium, and omega-3s, helping regulate sleep cycles.
- Fatty Fish (Salmon, Tuna, Mackerel) – High in omega-3 fatty acids and vitamin D, promoting serotonin production.
- Kiwi – Contains serotonin, which helps regulate sleep patterns.
- Chamomile Tea – Known for its calming properties and ability to improve sleep quality.
- Pumpkin Seeds & Nuts (Cashews, Pistachios, Sunflower Seeds) – Packed with magnesium, essential for relaxation.
- Bananas – Rich in magnesium and melatonin, naturally aiding sleep.
- Warm Milk & Golden Milk – Contains tryptophan, calcium, and vitamin D, promoting restful sleep.
- Whole Grains (Brown Rice, Quinoa, Whole Wheat Bread) – Magnesium-rich foods that help relax the body.
- Leafy Greens (Spinach, Kale, Collard Greens) – Contain magnesium for muscle relaxation and improved sleep.
- Berries (Blueberries, Strawberries, Raspberries) – Loaded with antioxidants and magnesium to enhance sleep quality.
Final Thoughts
Improving sleep hygiene and incorporating sleep-friendly foods can significantly reduce insomnia. Maintaining a healthy lifestyle, balanced diet, and stress management techniques can also promote better sleep quality. If insomnia persists, consulting a healthcare provider is recommended.
For more sleep health tips and expert advice, stay tuned to Nutriewind – your go-to source for sleep wellness and holistic health!

Nutrition
What is Thyroid Gland & Its Functions?
The thyroid gland is a small butterfly-shaped organ located in the neck, responsible for producing essential hormones like thyroxine (T4) and triiodothyronine (T3). These hormones regulate metabolism, energy production, and growth, affecting nearly every cell in the body. Proper thyroid function is vital for maintaining healthy weight, mood, and body temperature. Imbalances in thyroid hormone levels can lead to conditions like hypothyroidism or hyperthyroidism, impacting overall health.

Thyroid and its Functions
Hypothyroidism:
What is Hypothyroidism?
Hypothyroidism is a condition where the thyroid gland doesn’t produce enough thyroid hormones. These hormones are essential for regulating metabolism, energy levels, growth, and development. Without adequate thyroid hormone production, individuals can experience various physical and emotional symptoms.
Causes of Hypothyroidism (Aetiology)
Several factors can lead to hypothyroidism, including:
- Autoimmune Thyroiditis (Hashimoto’s Thyroiditis): The immune system attacks the thyroid gland.
- Thyroid Surgery or Radiation Therapy: Can damage the thyroid gland.
- Thyroid Gland Damage or Inflammation: Caused by infections, tumors, or cysts.
- Iodine Deficiency: Lack of iodine in the diet can prevent thyroid hormone production.
- Medications: Certain drugs like lithium and amiodarone can affect thyroid function.
- Pituitary Gland Disorders: Reduced thyroid-stimulating hormone (TSH) production can impact thyroid function.
Common Hypothyroidism Symptoms
- Fatigue & Weakness: Feeling tired despite adequate rest.
- Weight Gain or Difficulty Losing Weight: Slow metabolism leads to weight gain.
- Cold Sensitivity: Increased sensitivity to cold temperatures.
- Dry Skin & Hair: Skin may become rough, and hair can become dry and brittle.
- Hair Loss: Thinning or shedding of hair.
- Constipation: Slowed metabolism affects digestion.
- Depression & Mood Swings: Affects emotional well-being.
- Muscle Aches & Stiffness: Generalized muscle pain.
- Irregular or Heavy Menstrual Periods: Particularly in women.
Diagnosis of Hypothyroidism
To confirm hypothyroidism, doctors rely on:
- Blood Tests: Measurement of TSH, free T4, and free T3.
- Thyroid Function Tests: Evaluation of thyroid hormone production.
- Imaging Tests: Ultrasound, CT scan, or MRI to visualize the thyroid.

Blood Tests of thyroid
Treatment Options for Hypothyroidism
- Thyroid Hormone Replacement: Levothyroxine (T4) or liothyronine (T3) are prescribed to normalize hormone levels.
- Combination Therapy: A blend of T4 and T3 may be used for some patients.
- Regular Monitoring: Ongoing tests to adjust medication dosage as needed.
Complications of Hypothyroidism
If untreated, hypothyroidism can lead to:
- Goiter: An enlarged thyroid gland.
- Heart Problems: High blood pressure, heart failure, or atherosclerosis.
- Mental Health Issues: Anxiety, depression, or cognitive decline.
- Infertility or Miscarriage: Can affect women’s reproductive health.
- Osteoporosis: Increased risk of bone fractures due to weakened bones.
Hypothyroidism Risk Factors
- Family History: A history of autoimmune thyroiditis or hypothyroidism increases risk.
- Age: More common in women over 50.
- Autoimmune Disorders: Conditions like type 1 diabetes, rheumatoid arthritis, or lupus.
- Radiation Exposure: Radiation therapy to the neck or head increases the risk.
- Thyroid Surgery: Any partial or total thyroidectomy increases risk.
Hypothyroidism Diet: Foods to Include and Avoid
Foods to Include:
- Iodine-rich Foods: Seaweed, kelp, iodized salt, fish, dairy products.
- Selenium-rich Foods: Brazil nuts, fish, turkey, and beef.
- Zinc-rich Foods: Oysters, beef, chicken, pumpkin seeds.
- Tyrosine-rich Foods: Lean meats, fish, eggs, dairy.
- Omega-3 Fatty Acids: Fatty fish, flaxseeds, walnuts.
Foods to Avoid:
- Soy Products: Can interfere with thyroid medication absorption.
- Cruciferous Vegetables: Broccoli, cauliflower, kale (cook to reduce the impact).
- Gluten: May worsen autoimmune thyroiditis.
- Processed Foods & Sugary Fats: These can contribute to weight gain.
Hyperthyroidism:
What is Hyperthyroidism?
Hyperthyroidism is a condition where the thyroid gland overproduces thyroid hormones, causing an accelerated metabolism and leading to various health issues.
Causes of Hyperthyroidism (Aetiology)
Hyperthyroidism can be triggered by several factors:
- Graves’ Disease: An autoimmune disorder that stimulates the thyroid to produce excess hormones.
- Toxic Multinodular Goiter: Several thyroid nodules produce excess hormones.
- Toxic Adenoma: A single thyroid nodule overproduces hormones.
- Thyroiditis: Inflammation of the thyroid gland causing hormone release.
- Excessive Iodine Intake: Consuming too much iodine can stimulate the thyroid.
- Thyroid Hormone Overdose: Taking excessive amounts of thyroid hormone medications.
Common Hyperthyroidism Symptoms
- Weight Loss: Despite increased appetite.
- Rapid Heartbeat: Palpitations or irregular heartbeat.
- Nervousness: Anxiety, irritability, and mood swings.
- Fatigue: Weakness and exhaustion.
- Heat Intolerance: Increased sweating and flushed skin.
- Menstrual Changes: Lighter or irregular periods in women.
- Enlarged Thyroid (Goiter): Visible swelling in the neck.
- Hair Loss: Thin, brittle hair.
- Skin Problems: Fragile skin or rashes.
Diagnosis of Hyperthyroidism
The diagnosis involves:
- Blood Tests: Measurement of TSH, free T4, and free T3 levels.
- Thyroid Function Tests: Assessment of thyroid hormone levels.
- Imaging Tests: Ultrasound, CT scan, or MRI.
- Radioactive Iodine Uptake Test: To evaluate how the thyroid takes up iodine.
Treatment Options for Hyperthyroidism
- Antithyroid Medications: Methimazole or propylthiouracil to reduce hormone production.
- Radioactive Iodine Ablation: Destroys thyroid tissue to reduce hormone levels.
- Surgery: Removal of part or all of the thyroid gland.
- Beta-blockers: To control symptoms like rapid heartbeat and anxiety.
Complications of Hyperthyroidism
- Thyroid Storm: A rare, life-threatening emergency that requires immediate treatment.
- Osteoporosis: Excessive thyroid hormone weakens bones.
- Heart Problems: Increased risk of atrial fibrillation, heart failure, or stroke.
- Eye Issues: Graves’ ophthalmopathy causes bulging or inflamed eyes.
Hyperthyroidism Risk Factors
- Family History: A history of Graves’ disease or thyroid issues increases risk.
- Autoimmune Disorders: Conditions like type 1 diabetes or rheumatoid arthritis.
- Iodine Imbalance: Both excess and deficiency can trigger thyroid problems.
- Age: More common in women under 40.
Hyperthyroidism Diet: Foods to Include and Avoid
Foods to Include:
- Iodine-rich Foods: Seaweed, kelp, iodized salt (in moderation).
- Omega-3 Fatty Acids: Fatty fish, flaxseeds, walnuts.
- Antioxidant-rich Foods: Fruits, vegetables, whole grains.
- Calcium-rich Foods: Dairy, leafy greens, and fortified plant-based milk.
Foods to Avoid:
- Excessive Iodine: Avoid large amounts of seaweed or kelp.
- Soy Products: May interfere with thyroid medication absorption.
- Gluten: Can worsen autoimmune thyroid conditions.
- High-Sugar & Fatty Foods: These contribute to inflammation and weight issues.

Nutrition
Irritable Bowel Syndrome (IBS): Symptoms, Causes, Diagnosis, and Treatment
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder that affects a significant percentage of the adult population globally, leading to recurring abdominal pain, bloating, and changes in bowel movements. IBS is considered a chronic condition, with symptoms varying from person to person, but it can be effectively managed with the right approach.
What is Irritable Bowel Syndrome (IBS)?
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder characterized by discomfort in the abdominal region, altered bowel habits, and bloating. Although the exact cause of IBS remains unclear, several factors are thought to contribute to its development, including genetic predisposition, gut motility abnormalities, stress, food intolerance, and hormonal changes.

IBS
Causes of IBS
While the precise cause of IBS is still unknown, there are several key factors that may trigger or worsen the condition, including:
- Abnormal Gut Motility: Disruptions in the way the intestines move and contract can contribute to IBS symptoms, such as diarrhea or constipation.
- Visceral Hypersensitivity: Heightened sensitivity of the gut to stimuli may result in abdominal pain and bloating.
- Stress and Anxiety: Emotional and psychological stress can exacerbate IBS symptoms or even trigger flare-ups.
- Hormonal Changes: Hormonal fluctuations, especially in women, can influence gut motility and contribute to IBS.
- Food Intolerance: Certain foods can irritate the gastrointestinal system and trigger IBS symptoms.
- Genetic Factors: A family history of IBS may increase the likelihood of developing the condition.
Common Symptoms of IBS
Symptoms of IBS can vary greatly between individuals. Common signs include:
- Abdominal Pain or Cramping: Pain that may be relieved by passing gas or bowel movements.
- Bloating and Gas: A feeling of fullness or distention in the stomach.
- Changes in Bowel Movements: Alternating diarrhea and constipation or chronic diarrhea or constipation.
- Mucus in Stool: The presence of mucus in the stool may indicate IBS.
- Incomplete Evacuation: The sensation of not fully emptying the bowels after a movement.
- Nausea and Vomiting: Digestive discomfort may lead to feelings of nausea.

How is IBS Diagnosed?
There is no definitive test for IBS, and diagnosis is primarily based on symptoms. The Rome IV criteria are widely used to diagnose IBS, which include:
- Recurring abdominal pain or discomfort at least once a week for the past three months.
- Pain associated with at least two of the following:
- Changes in stool frequency (more or less frequent than usual).
- Changes in stool form (loose, hard, or lumpy).
- Changes in stool appearance (mucus or abnormal color).
A healthcare provider will also consider medical history, conduct a physical examination, and may run tests to rule out other gastrointestinal disorders.
Treatment Options for IBS
IBS treatment typically involves a combination of lifestyle modifications, dietary changes, and medications to manage symptoms effectively.
Lifestyle Modifications
- Stress Management: Stress reduction techniques, including yoga, meditation, or deep breathing exercises, can alleviate IBS symptoms.
- Regular Exercise: Physical activity can improve gut motility and reduce symptoms like constipation.
- Adequate Sleep: Good sleep hygiene plays a key role in managing stress and improving overall health.
- Avoiding Trigger Foods: Identifying and eliminating foods that exacerbate IBS symptoms is essential for long-term relief.
Medications
Medications may be prescribed to manage specific symptoms, such as:
- Antispasmodics: To alleviate abdominal pain and cramping (e.g., dicyclomine).
- Antidepressants: Low-dose antidepressants like amitriptyline can help reduce pain and improve bowel function.
- Laxatives: To relieve constipation (e.g., senna).
- Anti-diarrheal Medications: To control diarrhea (e.g., loperamide).
Dietary Changes for Managing IBS
Diet plays a significant role in managing IBS symptoms. A personalized diet plan, developed with the guidance of a healthcare provider or registered dietitian, is highly recommended. Some general dietary guidelines include:
- Eat Smaller, Frequent Meals: Smaller meals help reduce bloating and discomfort.
- Avoid Trigger Foods: Common IBS triggers include gluten, dairy, spicy foods, and processed foods.
- Increase Fiber Intake: Foods high in fiber, such as fruits, vegetables, and whole grains, can improve bowel movements.
- Stay Hydrated: Drinking plenty of water is important, especially if experiencing diarrhea.
The FODMAP Diet for IBS Relief
The FODMAP diet is an evidence-based dietary approach that has shown promise in reducing IBS symptoms. FODMAPs are certain types of carbohydrates that can be difficult for some people to digest, leading to symptoms like bloating, gas, and abdominal pain.
The FODMAP diet includes three phases:
- Elimination Phase: Remove high-FODMAP foods for 2-6 weeks to assess symptom improvement.
- Reintroduction Phase: Gradually reintroduce high-FODMAP foods one at a time to identify specific triggers.
- Modification Phase: Develop a personalized eating plan that minimizes or avoids trigger foods.
Common high-FODMAP foods to limit or avoid include:
- Wheat, barley, and rye (fructans)
- Onions, garlic, beans, and soybeans (fructans and galactans)
- Apples, pears, watermelon, and mangoes (fructose)
- Dairy products, especially those high in lactose
- Sorbitol, mannitol, and xylitol (polyols)

IBS- Irritable Bowel Syndrome
Risk Factors for IBS
Several factors increase the likelihood of developing IBS, including:
- Family History: A genetic predisposition may increase your risk.
- Stress and Anxiety: Psychological stress can trigger or worsen IBS symptoms.
- Hormonal Changes: Hormonal shifts, especially in women, can affect gut function.
- Food Intolerance: Sensitivity to certain foods can contribute to IBS.
- Infections: Gastrointestinal infections may increase susceptibility to IBS.
- Neurological Disorders: Conditions like Parkinson’s disease may also raise IBS risk.
Conclusion
If you’re struggling with IBS, working with a healthcare provider and making targeted lifestyle and dietary changes is essential for effective management. With the right approach, you can significantly reduce symptoms and improve your quality of life. IBS is a manageable condition, and with personalized care, it’s possible to find a treatment plan that works for you. Always consult a healthcare professional or registered dietitian before making significant changes to your diet or lifestyle.

Nutrition
The Health Benefits of Eating Banana Slices with Milk: A Nutritious Snack or Breakfast
Eating banana slices with milk is a delicious, quick, and nutrient-packed way to enjoy this simple combination. The milk adds a creamy texture and a mild flavor that complements the natural sweetness of bananas. Whether you enjoy it as a snack or a breakfast, this pairing is a convenient and satisfying choice for those looking for a healthy, energy-boosting option.

The Health Benefits of Eating Banana Slices with Milk
Nutritional Benefits of Bananas and Milk
Bananas are rich in potassium, fiber, and essential vitamins, while milk is packed with calcium, protein, and vitamin D. Together, they create a well-balanced snack that supports overall health. You can also customize your banana and milk combination by adding a sprinkle of cinnamon, a drizzle of honey, or a handful of nuts to boost flavor and texture.

The Health Benefits of Eating Banana Slices with Milk: A Nutritious Snack or Breakfast
Who Can Benefit from Eating Banana Slices with Milk?
- Growing Children: The combination of milk and bananas provides essential nutrients like calcium, potassium, and vitamins that are crucial for growth and development.
- Athletes and Active Individuals: This snack is a great source of quick energy, potassium for muscle function, and protein for recovery, making it perfect for athletes or anyone with an active lifestyle.
- Those with Potassium Deficiency: The potassium in bananas helps replenish this vital nutrient, which is essential for heart and muscle function.
- Individuals Seeking a Healthy Snack: For those looking to maintain a balanced diet or manage their weight, banana slices with milk provide a satisfying, nutrient-dense snack that helps curb hunger.
- Pregnant or Breastfeeding Women: Bananas and milk offer essential nutrients like calcium, vitamin D, and potassium that are important for fetal development and milk production.
- People with Digestive Issues: The potassium in bananas helps soothe digestive issues, and the probiotics found in milk can support a healthy gut.
- Individuals with High Blood Pressure: Potassium is known to help regulate blood pressure, and the high potassium content of bananas makes them beneficial for individuals with high blood pressure.
- Those with Muscle Cramps or Spasms: The combination of potassium and magnesium in bananas can help alleviate muscle cramps, making it a great snack for those prone to muscle spasms.
- Pre- or Post-Workout Snack Seekers: Banana slices with milk provide the ideal balance of carbohydrates, potassium, and protein, supporting muscle function and replenishing energy before or after exercise.
- Those Looking for a Comforting, Easy-to-Digest Food: If you’re seeking a soothing snack that is gentle on your stomach, banana slices with milk can be a perfect choice for a comforting and easily digestible option.
Conclusion: A Nutrient-Rich Pairing
Banana slices with milk are not only a delicious and satisfying snack but also a powerhouse of essential nutrients. Whether you’re looking for a quick energy boost, a healthy snack, or a way to support your health goals, this easy combination offers numerous benefits. So, next time you’re craving a nutritious treat, reach for some banana slices and milk!